Herniated Disc and Sciatica
Treatment for herniated disc
Is it possible to efficiently treat patients with herniated discs without surgery?
A healthy spine is made up of stacked bones that are vertebrae, muscles, tendons, ligaments, nerve roots and intervertebral discs. This is what healthy intervertebral discs look like, located between the vertebrae. Over time, use and wear, disc herniations occur.
Disc herniation can occur in any intervertebral disc, but is most common in the lumbar spine. Symptoms of a herniated disc can vary depending on the severity of the hernia and its location. The interaction of inflammatory substances from the herniated disc with nerves can cause pain due to inflammatory chemical irritation. However, we must also consider the possibility of direct compression of the nevus roots by disc protrusion, which can promote neuritis or inflammatory nerve injury.
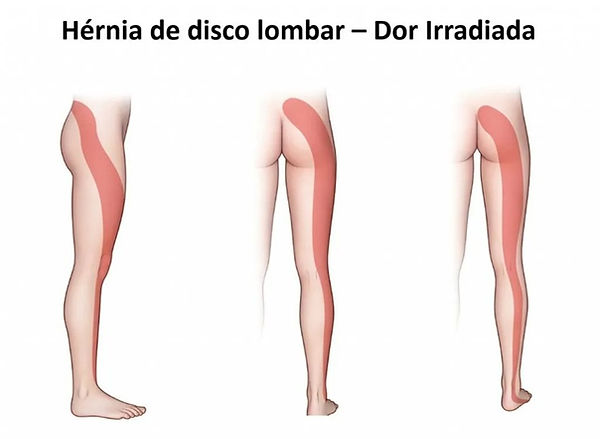
Disc herniation can cause a range of symptoms, such as local pain when it does not generate nerve compression, to neurological symptoms, generating loss of function of the compressed nerve, lack of strength, sensitivity and radiating pain. Pain radiating along the path of the nerve is what characterizes sciatica, or lumbar radiculopathy, also causing symptoms in the legs.
Many patients think that treatment for herniated discs must be surgical to be effective. Herniated disc surgery is only indicated in 5% of cases, but experts recognize that there is an excess of operations, which could affect up to 40% of patients. Some studies indicate that if a patient with a herniated disc first consults a surgeon, he or she is much more likely to resort to surgical treatment, which in most cases may be unnecessary.
Furthermore, a treatment that involves some risks and complications during the operation, such as infections, anesthesia and also a post-operative period that can be more complex depending on the surgical technique.
Therefore, surgical treatment should only be adopted when all other treatments do not produce satisfactory results or when there is an immediate risk of permanent injury.
But what is the conservative treatment to be adopted? Physiotherapy, chiropractic?
Not all professionals on the market are prepared to treat herniated discs. There are professionals and services duly specialized in the non-surgical treatment of herniated discs. This treatment must be focused on biomechanics, controlling pain and inflammation and mainly on decompressing the herniated disc.
Preferable movements and positions must be observed to preserve the integrity of the nerves.
Flexodistraction using the COX table produces decompression during the course of treatment that allows rehydration of the disc and release of the nerve root without the need for surgery.
Spinal decompression is a safe non-invasive technique capable of making a decisive contribution to the treatment of herniated discs.
The association of medications, physical equipment such as laser and other anti-inflammatory equipment are associated with flexodistraction decompression.
This makes it possible to achieve at least partial regression of the herniated disc and resolution of symptoms. The Vertebral Column Institute now has the COX TABLE, for the conservative treatment of DISC HERNS. Always innovating to better serve our patients.
Before deciding to undergo surgery for a herniated disc, it is very important to go as far as possible with conservative treatment.
What is Flexo-distraction?
Flexion-distraction is a technique developed by American chiropractor J. Cox D.C (Flex Distraction Cox Technic) for the treatment of various spinal conditions, mainly herniated discs, low back pain and scoliosis.
The Traction Table provides stretching (decompression) of the discs and soft structures of the spine (ligaments and muscles), reducing intradiscal pressure, and facilitating the flow of fluids and nutrients to the disc, reactivating the disc's metabolism.
Indications for Flexodistraction:
1. Disc herniation
2. Chronic low back pain
3. Sciatica
4. Degenerative stenosis
5. Osteoarthritis
WHEN DO DISC HERNIATIONS OCCUR?
Disc herniations occur when there is some level of displacement or volume of the vertebral disc, due to loss of integrity of its histological structure. Intervertebral discs are structures existing between each vertebra with the aim of generating mobility and stability between each bone in the spine. In some cases, biomechanical stress, among other environmental factors, leads to damage to the internal rings of intervertebral discs and changes in the mobility of the vertebral segment, which can cause compression of nerve roots, causing pain and disability.

A herniated disc can generate different symptoms, depending on the segment of the spine that is affected. If it occurs in the lumbar spine, it generally causes symptoms in the legs, and if it occurs in the neck region (cervical spine) it can cause pain in the neck, radiating pain in the arms, pain in the shoulders and numbness or tingling in the arms or hands. Thus, a herniated disc may compromise the function of the peripheral nervous system, leading to sciatica or cervicobrachialgia. Cervicobrachialgia is a condition of pain in the cervical region that is distributed throughout the upper limbs, caused by nerve compression in the cervical region.
In general, a herniated disc causes symptoms for 4 to 6 weeks and if it does not lead to radicular compression (compression of the nerves leaving the spine), it will not have major consequences for the patient.

Types of Disc Herniation
Disc bulging: Disc bulging is the first characteristic phase of disc herniation, indicating an initial degree of degeneration of the disease. One of the main causes of the problem is aging, that is, the process of degeneration caused by the rupture of the fibers of the fibrous ring.
Disc protrusion: This is the most common type and is characterized by the fact that the nucleus of the disc enlarges, but remains intact, although it has already lost its oval shape. And, due to the enlargement, the walls of the disc may touch regions and areas of great nervous sensitivity, causing pain and inability to perform some movements.
Extruded disc herniation: This case is serious, as the nucleus of the disc is already deformed, fragmented to the point where the nucleus pulposus completely loses its original shape and looks like a “drop”. When the disc ruptures, the gelatinous liquid escapes through a crack in the membrane, losing contact between the fragments and their internal environment.
Sequestered disc herniation: This type is even more serious, because the disc is already so damaged that it can split in half. When this rupture occurs, the gelatinous liquid enters the spinal canal and presses on the nerve root, causing continuous compression and inflammation. This type of hernia is what causes the so-called “chemical pain”, because when the gelatinous liquid is outside its natural environment, its acidic chemical properties cause unbearable pain.

Can herniated discs regress?
The answer is yes and the larger the hernia the greater the chance of regression.
Kidnapping – 96%
Extrusion – 70%
Protrusion – 41%
Degeneration – 13%
Some studies indicate that the regression of extruded hernias is 15% and that of sequestered hernias is 43%. It doesn't seem like much, but it's enough to stop causing disabling symptoms, such as pain.
Of course, these data change in different studies, depending on the population, as there are genetic and environmental issues linked to each population. In the United Kingdom, this percentage is 82.94%. In Japan it is 62.58% and, overall (from the study), the regression rate for herniated discs is 66.66%.

Symptoms:
1. Back pain for more than three months;
2. Back pain during nighttime sleep, which remains when waking up;
3. Difficulty sitting correctly (upright spine) for more than 10 minutes;
4. Weakness in one or both legs;
5. Tingling, pain or numbness in the arms and legs;
6. Inability to stand on one leg;
7. Extreme difficulties holding urine;
8. Reduced income and discouragement in carrying out routine activities;
9. Headaches associated with pain in the back of the neck, which extends to the shoulders;
10. Difficulties moving around or lifting an object.

Sciatica and Disc Herniation
Sciatica consists of pain in the sciatic nerve. This typically results from compression of the lumbar nerve roots in the lower back. The most common is sciatica due to a herniated disc, which is located in the lumbar region. This hernia effectively generates compression on the lumbar roots that form the sciatic nerve.
Common causes include discopathies, osteophytosis and narrowing of the spinal canal (medullary stenosis). Symptoms are radiating pain from the gluteal region running along the back of the lower limb to the foot. Diagnosis is made by MRI or CT. Electromyography and nerve conduction studies help confirm the affected level. Treatment is symptomatic and, sometimes, surgery, particularly if there is a neurological deficit.
Medial and Lateral Disc Herniation: SHIFT
Lateral deviation (also called “lateral shift”) can be explained as a mechanism (active or reflex) used to avoid compression or irritation of a certain innervation through mainly muscle spasms and contractures. Patients who fall into this group receive lateral deviation exercise techniques to correct the deviation and are also directed to mechanical traction or self-traction.
As a clinical presentation, the patient who fits into this group presents as characteristics the clear deviation in the frontal plane of the shoulders in relation to the pelvis and the preference for lateral translation movements (displacement) of the pelvis. Lateral deviation can be to the left or right and can be toward the dominant side of pain (ipsilateral) or away from the side of pain (contralateral). Most affected patients have a contralateral deviation.
Treatment
Here at Instituto Coluna Vertebral, through 20 years of clinical experience, we have developed a multimodal protocol combining different resources and very special clinical management to achieve the best results for Herniated Discs.

Ilustração do shift - Posição antalgica do paciente
.png)